Victoria Stiller

Victoria Stiller
Former MD Student
Medical Doctor Project 4
MD4: Investigating the mode of mast cell-driven translation of local inflammation into systemic effects — impact mobilization or emergency myelopoiesis?
|
|
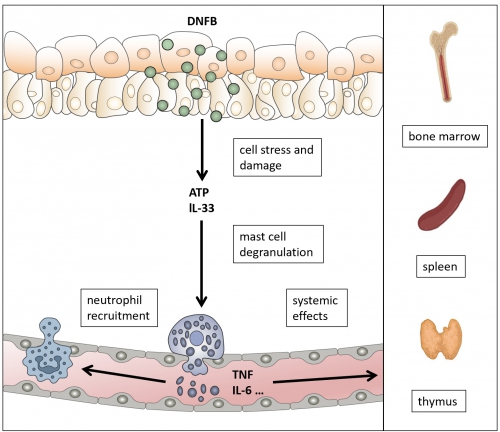
Mast cells (MCs) are long-lived immune cells that predominantly reside in tissues at interfaces with our environment. In particular, they function as sentinels, e.g. in the connective tissue of the skin and in the mucosae, and contribute to acute host defense. We found that in contact hypersensitivity (CHS), a mouse model of human allergic contact dermatitis, MCs sense the keratinocyte cell stress mediators ATP and Interleukin (IL-) 33. The resulting MC degranulation induces vascular responses and neutrophil recruitment. Importantly, perivascular MCs are able to cross the endothelial barrier, form intraluminal sheets and degranulate directionally into the bloodstream upon inflammatory insult. Tumor necrosis factor (TNF), contained in these granules, was found responsible for priming blood neutrophils. Consequently, we hypothesize that MCs can initiate systemic effects upon local inflammation, for example by releasing several proinflammatory cytokines and chemokines, such as TNF and IL-6 . To address this hypothesis, we will investigate the impact of MC depletion on I) the release of humoral components of innate immunity (acute phase proteins, cytokines, chemokines), II) immune cell mobilization from the bone marrow (BM), spleen, and thymus and III) the perivascular BM-resident dendritic cell (DC) subsets involved in progenitor mobilization. By comparing local and systemic MC depletion, we will discriminate the role of skin resident MCs from the functions of MCs in the target organ, e.g. spleen and BM. Moreover, by examining the kinetic of MC effects, we will clarify whether MCs predominantly induce cell mobilization from distant organs, or affect the subsequent restoration of the cell pool by emergency myelopoiesis.
The contact hypersensitivity model and intravascular degranulation of perivascular MCs. Epicutaneous application of DNFB triggers keratinocyte cell stress and release of ATP and IL-33. MCs respond by degranulation, thereby inducing vascular responses and neutrophil recruitment. Mechanistically, we found that perivascular MC degranulate directionally into the bloodstream, which, beyond neutrophil recruitment, may cause systemic effects. |
Photos: by UMMD, Melitta Schubert/Sarah Kossmann