Jonas Negele

Jonas Negele
Medical Doctor Project 7
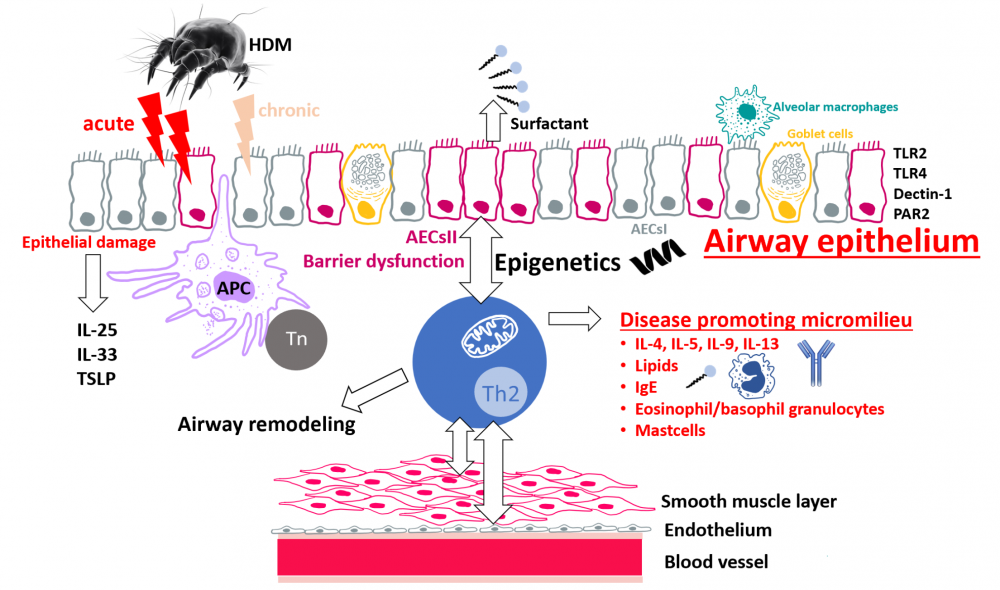
MD7: Epigenetic perpetuation of chronic asthma in airway epithelial type II cells
|
|
The development of allergic asthma is associated with specific genetic risk factors, smoking and obesity. Currently, allergic asthma affects approximately 300 million people worldwide, which creates a significant burden to our healthcare system. The disease pathogenesis involves the sensitization and reexposure to environmental allergens such as animal hair, pollen or components of house dust mites (HDM). During chronic asthmatic airway inflammation, the lung microenvironment, which is evoked by the cellular crosstalk of T helper (Th)2 cells and the airway epithelium including airway epithelial type II cells (AECsII), induces a barrier dysregulation, goblet cell metaplasia/hyperplasia, subepithelial fibrosis, increased endothelial permeability and smooth muscle cell thickening. In our project we hypothesize that the specific disease-promoting microenvironment during asthmatic airway inflammation alters the airway epithelial barrier and mediates the perpetuation of chronic lung inflammation by epigenetic mechanisms in AECsII. To experimentally address this question, we induce acute and chronic HDM-induced asthmatic airway inflammation in mice to ultimately study the mechanisms of chronic epigenetic fixation of the disease in AECsII by ATAC sequencing. In addition, we seek to unravel the intracellular signaling pathways in AECsII that are involved during the establishment of chronic allergic lung inflammation. Pathogenesis of HDM-induced asthma. Protease-containing HDM sensitize the airway epithelium via TLR2, TLR4, Dectin-1 and PAR2 and cause epithelial damage. Airway epithelial cells secrete the epithelial-derived factors IL-25, IL-33 and TSLP, so-called alarmins, which initiate type 2 immunity, due to activation of APCs. Naïve T cells differentiate to Th2 cells and migrate to the subepithelial layer. By the production of type 2 cytokines (IL-4, IL-5, IL-9 and IL-13) Th2 cells recruit eosinophils and induce isotype switch and thus IgE production. The disease-promoting milieu cumulates in an epithelial barrier dysfunction and epigenetic fixation of the chronic lung disease. The latter and the intracellular signaling events in airway epithelial cells that are involved in these processes will be investigated in this project. Abbreviations: AECsII, Airway epithelial type II cells; APC, Antigen-presenting cell; HDM, House dust mites; IgE, Immunoglobulin E; IL, Interleukin; PAR, Protease-activated receptor; Th2 cell, T helper 2 cell; TLR, Toll-like receptor; Tn, naïve T cell; TSLP, Thymic stromal lymphopoietin. |
Photos: by UMMD, Melitta Schubert/Sarah Kossmann