|

PhD Student

Project Leader
|
|
Biliary tract cancer, also known as cholangiocarcinoma (CCA9, accounts for about 2% of all malignancies, but incidences of intrahepatic CCA are rising and prognosis of CCA is dismal with surgical resection or liver transplantation as only curative treatment options. Chronic inflammation of the bile ducts and surrounding portal fields are a hallmark of CCA pathogenesis. Chronic diseases of the intra- and extrahepatic bile ducts, such as primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC) predispose to CCA development. Bile acids (BAs) play a fundamental role in both liver damage and regeneration. BA effects are mediated through different receptor molecules, comprising nuclear BA receptors (BARs) and G protein-coupled receptors (GPCRs), such as the Takeda G protein-coupled receptor-5 (TGR5, GPBAR1) or the sphingosine 1-phosphate receptor-2 (S1PR2). While secondary BAs have been shown to impair epithelial barrier function in different epithelial cells through disruption of tight junction integrity, BARs such as TGR5 can protect epithelial cells at the interface with bile through increased bicarbonate secretion and phosphorylation and stabilization of tight junction and adhesional molecules.
TGR5 is expressed in biliary epithelial cells (BECs, cholangiocytes) throughout the biliary tree including the extrahepatic duct as well as the gallbladder both in humans and rodents. TGR5 is localized both in the apical membrane and in the primary cilium which represent the interface of BECs with bile. Previously, we identified an essential role of TGR5 and TGR5-dependent signaling for BA-induced BEC proliferation. Besides proliferation, TGR5 protects BECs from BA toxicity and preserves integrity of the epithelial barrier. The mechanisms contributing to this protective effect comprise anti-apoptotic signaling, strengthening of tight junction integrity and increased chloride and bicarbonate secretion. The latter contributes to the formation of the so-called „bicarbonate umbrella”, which shields the biliary epithelial barrier from the detergent activity of biliary BAs. Absence of TGR5 in mice was associated with a maladaptation to injury resulting in aggravated biliary injury, reduced compensatory biliary proliferation, increased portal pressure, rapid development of liver fibrosis. In line with these findings, we observed a disease and cell-type specific downregulation of TGR5 in BECs from patients with PSC, a rare cholestatic liver disease characterized by chronic inflammation and progressive fibrosis of the intra- and extrahepatic bile ducts. Mice lacking the hepatocyte phospholipid floppase Abcb4 recapitulate the progressive fibrosing cholangitis aspect of human PSC and also develop intrahepatic malignancy. We recently described that reduction of TGR5 in BECs of Abcb4-/- mice triggers development of the inflammatory, reactive BEC phenotype typical for sclerosing cholangitis as demonstrated by single-cell RNA-sequencing. In contrast, overexpression of TGR5 abolished the reactive BEC phenotype, which could also be achieved by norUDCA feeding. The latter was associated with normalization of TGR5 expression in BECs of Abcb4-/- mice. We thus identified a hitherto unknown mode of action of norUDCA, which is currently tested in a phase III clinical trial for PSC. In addition to TGR5, BECs and immune cells also express S1PR2. While liver injury was aggravated in TGR5-/-, knockdown of S1PR2 ameliorated liver damage. The extent to which the functions of these two BARs overlap and in which aspects their role differs in BECs is yet unclear. Moreover, the interplay of TGR5 and S1PR2 in different liver cells during cholestasis is incompletely understood. Both TGR5 and S1PR2 are druggable targets with a variety of potential applications in liver diseases. A better understanding of the regulation, function and interaction of TGR5 and S1PR2 in BECs and adjacent immune and matrix cells under physiological and biliary disease conditions is the central aim of the project. We hypothesize that both TGR5 and S1PR2 contribute to BEC barrier function and that maladaptation of the crosstalk and the mutual interdependence of these BARs in BECs and surrounding immune cells and myofibroblasts in response to injury results in biliary disease.
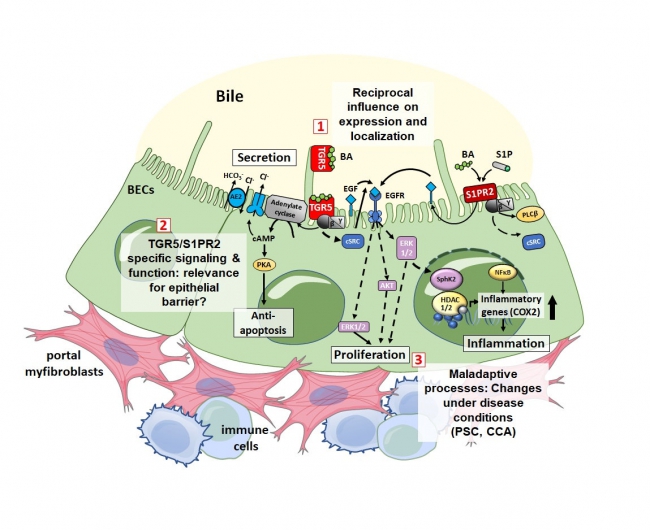 Mechanisms of interplay of TGR5 and S1PR2 for BEC barrier function under physiological and disease conditions. TGR5 and S1PR2 are both highly expressed in BECs and exert overlapping synergistic but also distinct function. Whether both receptors contribute to BEC barrier function is unknown. Furthermore, their role for maladaptive processes and inter-cellular communication (e.g. with myofibroblasts and immune cells) following biliary injury have not been elucidated. Mechanisms of interplay of TGR5 and S1PR2 for BEC barrier function under physiological and disease conditions. TGR5 and S1PR2 are both highly expressed in BECs and exert overlapping synergistic but also distinct function. Whether both receptors contribute to BEC barrier function is unknown. Furthermore, their role for maladaptive processes and inter-cellular communication (e.g. with myofibroblasts and immune cells) following biliary injury have not been elucidated.
|









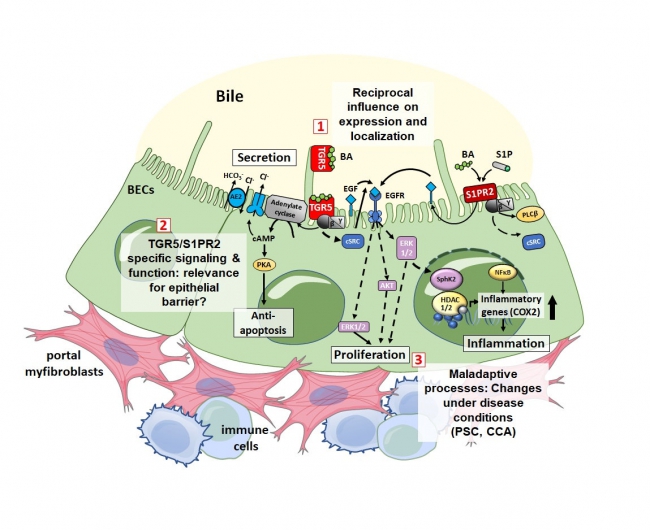 Mechanisms of interplay of TGR5 and S1PR2 for BEC barrier function under physiological and disease conditions. TGR5 and S1PR2 are both highly expressed in BECs and exert overlapping synergistic but also distinct function. Whether both receptors contribute to BEC barrier function is unknown. Furthermore, their role for maladaptive processes and inter-cellular communication (e.g. with myofibroblasts and immune cells) following biliary injury have not been elucidated.
Mechanisms of interplay of TGR5 and S1PR2 for BEC barrier function under physiological and disease conditions. TGR5 and S1PR2 are both highly expressed in BECs and exert overlapping synergistic but also distinct function. Whether both receptors contribute to BEC barrier function is unknown. Furthermore, their role for maladaptive processes and inter-cellular communication (e.g. with myofibroblasts and immune cells) following biliary injury have not been elucidated.